“I am happy now that I know what the problem is:” Braving to carry triple burden of HIV, cervical cancer and Female Genital Schistosomiasis.
Introduction
“The foul smell forces me to bathe at least twice a day. If I’m on a safari, I must put on pads so that it doesn’t leak out. The discharge is not pleasing at all. I fear being where people are gathered because of the smell. Most often, I don’t have sexual intercourse with my partner because I feel ashamed, though he has never complained. I have had this discharge and abdominal pains since August 2024 and visited two health facilities where I was given drugs to take with my spouse, but these did not relieve the pains and the discharge. I have also taken herbal medicine since I thought it could be rariew (a Luo word for lower abdominal pain experienced by women of reproductive age that is believed to be associated with growth covering the cervical opening which can prolapse to the vaginal opening if left untreated).” These were Caren’s* words when I met her during FGS-SRH Outreach. Her eyes and voice said it all. She looked and sounded sad as she told her story.
Integrating Female Genital Schistosomiasis and Sexual and Reproductive Health Activities along Lake Victoria region
The Ministry of Health-Homa Bay County in collaboration with LVCT Health and Frontline AIDS has been integrating reproductive health outreaches with services, such as HIV testing, cervical cancer screening, and Female Genital Schistosomiasis (FGS) screening, diagnosis, and treatment. The outreaches aim at reaching populations that are vulnerable to FGS like the fisherfolk community who live and work along Lake Victoria’s beaches. Human activities along the lake like fishing, bathing, swimming, washing clothes, and drawing water for domestic use also puts them at risk of getting infected with parasites that cause urinary schistosomiasis. Both men and women (young and old) are at risk of getting infected.
Caren’s painful journey of unknowing having FGS and cervical cancer on top of her known HIV status
I met Caren, a fishmonger, during one of the outreaches where we integrated the management of FGS) and sexual reproductive health (SRH) along the beaches of Lake Victoria in Homa bay County. As we screened her for risk of FGS we requested her to allow us to conduct a pelvic examination to diagnose FGS in a tent we had pitched on the beach. She was hesitant at first but she consented after we provided information about the pelvic examination. “Sister (to mean nurse), I am very happy today because you have brought the services closer to me. I have suffered…” she said as we prepared to proceed with the pelvic examination. Caren has lived with HIV since 2015 and she depends on Lake Victoria for her entire livelihood.
Adding two more diagnoses to Caren
As she undressed and positioned herself on the couch for the pelvic examination, a noticeable odour hung in the room. Her inner garment had a dark stain and the discharge appeared dark brown. As I guided her to assume the lithotomy position, she turned to me worriedly and asked “sister utaweza, ninanuka sana” [nurse, will you bear the smell, I smell a lot]. I reassured her not to worry and that our team was there to ensure she received the best care.
The pelvic exam using a speculum revealed that her cervical opening was completely covered with lesions and was discharging pus. The blood vessels were engorged and bled easily on contact. She also had rubbery polyps on the anterior wall of her cervix. We confirmed she had FGS and a possible case of cervical cancer. Given her weight, we prescribed five tablets of praziquantel to be taken after meals. We also advised her to visit the Homabay County referral hospital for a cervical cancer examination. We also linked her to health care providers at her local primary health facility for continued anti-retroviral treatment (ART). Despite receiving two diagnoses, Caren left the examination tent in high spirits. “Now I know clearly what the problem is, and I am going to share with my husband…” she said as she left the tent.
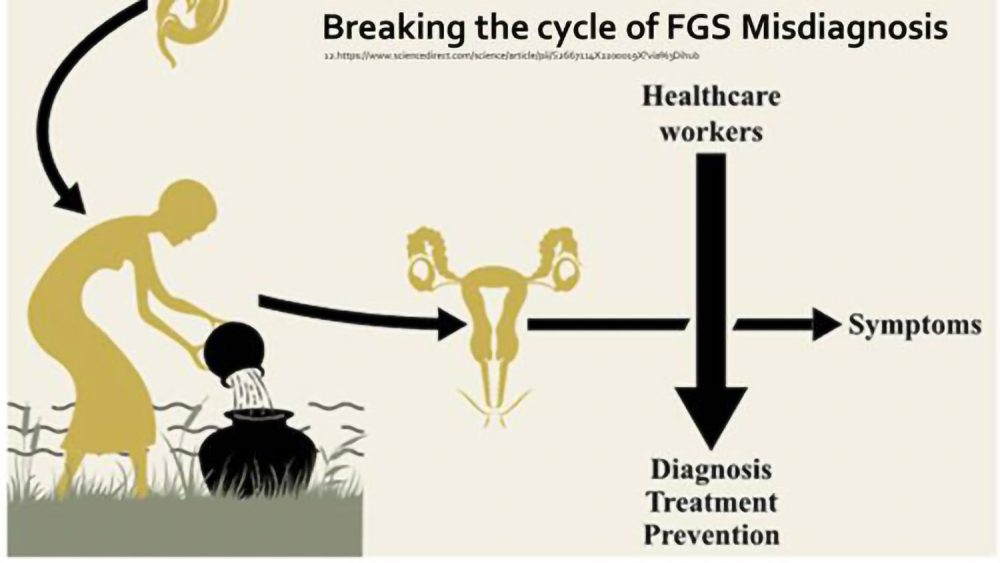
Genital schistosomiasis is caused by chronic inflammation of urogenital tissues when eggs of Schistosoma haematobium are lodged in the walls of the urogenital tract. In females, this inflammation primarily occurs in the vaginal and cervical walls. FGS is often misdiagnosed as a sexually transmitted infection or cervical cancer. Males with genital schistosomiasis experience inflammation in the seminal vesicles, prostate gland, and other structures of the male reproductive tract, including the vas deferens.
This experience with Caren, and other women, underscores the importance of integrating FGS and routine SRH services. Caren’s case is just a tip of an iceberg, highlighting the burden of FGS in the Lake Victoria region, particularly among the fisherfolk community. Due to their demanding daily lives, community members rarely seek medical attention for ‘minor’ ailments such as lower abdominal pains or genital itchiness. Many only seek medical attention when their condition worsens.
To bridge this gap, mobile clinics and outreach programs are urgently needed, rather than relying solely on facility-based care. Additionally, it will be critical to train more health workers on how to identify and manage FGS, not in isolation, but through an integrated model that efficiently addresses the region’s three major threats: HIV, Cervical cancer and FGS.
Call to action
FGS must be recognized as a serious public health problem that requires dedicated funding and integrated interventions. An opportunity lies in revising health workers training curricula to ensure that clinical screening and diagnosis are included.
Let us Unite, Act and Eliminate FGS
*Name changed for confidentiality purposes.
Story written by Millicent Ouma. Millicent is a Senior Research Officer at LVCT Health. Millicent holds a Bachelor of Arts Sociology and Anthropology and Diploma in Nursing.